The hospital’s emergency operations plan includes written procedures for when and how it will shelter in place or evacuate (partial or complete) its staff, patients, and volunteers.
Note 1: Shelter-in-place plans may vary by department and facility and may vary based on the type of emergency or situation.
Note 2: Safe evacuation from the hospital includes consideration of care, treatment, and service needs of evacuees, staff responsibilities, and transportation.
SHELTER IN PLACE
There has been an increasing prevalence of compound incidents (simultaneous, cascading, or regional incidents). Furthermore, recent research points to more rapid intensification of major storms in the Atlantic basin (Trends in Global Tropical Cyclone Activity: 1990–2021, Philip J. Klotzbach et al.) – providing less time for evacuation planning and decision making. Consequently, options to evacuate patients are decreasing. UTMB is therefore developing strategies to improve options for sheltering in place with patients who are unable to be evacuated (e.g., due to time constraints, medical constraints, et cetera).
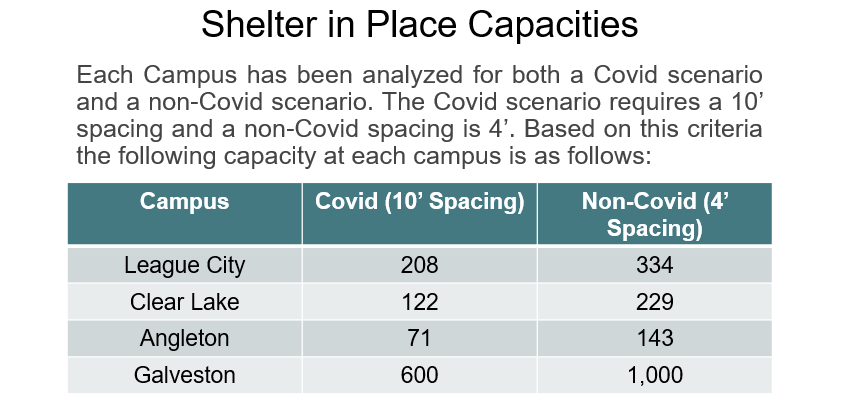
Toward this end, UTMB has invested considerable resources and effort in developing staff shelters at each campus. The Staff Shelter Plan is managed by the Support Division within the Logistics Section of the UTMB Institutional Command Team.
The total number of patients sheltering will be used to calculate the number of healthcare and support staff (typically between 800-1000) that will staff the ride out. Cots and linens are on hand to use in staff shelters; and spacing will be decided by Infection Control pending any ongoing disease outbreak. Generally two 12-hour shifts will be used so that around the clock care will be available. Staff members supporting healthcare staff are also included. Generally, four food servings will be offered using a fixed menu (so that each shift has the opportunity to have three meals).
Ride out staff will be identified on a HICS Organizational Assignment Form (or comparable document or information system). If at all possible, the Ride out Team will be released from work prior to landfall in order to prepare their families/homes
for the hurricane – and they will be given a time and date to report for their Ride out assignment. The Relief/Damage Assessment/Recovery Team will be released prior to landfall and provided a communications plan to initiate their return
to campus post-storm.
UTMB has a plan to close down non-mission essential buildings during the storm (see campus emergency planning maps in EM.12.02.11 EP1). The Health System Shelter Team will remain in the healthcare core buildings. Other teams will be assigned based on critical mission
such as animal care, utilities, facilities, et cetera.
Force Account Labor tracking should include the location and assignment of all staff members during working hours. Off duty shifts will check into and out of staff shelters in order to maintain accountability. Managers must maintain staff accountability
during the rideout – meaning that the location of every staff member is known and tracked through the entire ride out until demobilization and arrival of the Relief Team.
More detailed information on internal and external resilience is located in UTMB's Hurricane Planning Presentation (authorized personnel only), which contains information on window glazing for flying debris, flood mitigation, power/water/sewer, emergency
maps, and et cetera.
EVACUATION
The Clinical Enterprise CEO or their designee will serve as the Clinical Enterprise Operations Chief when the Institutional Command Team is activated – or as the Incident Commander of the Clinical Enterprise Incident Command. This position is responsible for
Patient Management and Evacuation. Planned evacuation will be coordinated with the Institutional Command Team Incident Commander.
UTMB has four hospital campuses and a large number of clinic locations. Alternate care sites are primarily in these UTMB controlled spaces. Evacuation/Relocation to these sites benefits from continuity of care, communications, and services provided.
The first choice will be to shift patients, medications, supplies, equipment, and staff to another facility within our organization.
- Communications: Existing phone and network communications will be used. Handheld radios are available if needed. For mass vaccination clinics at facilities owned by partnering agencies, UTMB Information Services will be part of the planning committee
and will develop a communications plan that could include secure remote network access for e.g. electronic medical records and state registries.
UTMB has established a Shelter in Place and Evacuation Plan for evacuation of UTMB hospitals or unit within a hospital. In the event the hospital or a unit is deemed unsuitable for continued occupancy or cannot support adequate patient care,
the Evacuation Plan will be initiated. Staff members are trained on evacuating both horizontally and vertically. Staff are also trained to request assistance in evacuating non-ambulatory patients and may also use the evacuation sleds and pediatric
evacuation vests or carriers if necessary.
The UTMB Fire Plan dictates that, in the event of a fire emergency, the initial preferred evacuation method will be horizontal evacuation to an area of safe refuge / an adjoining smoke-free compartment. If evacuation from the facility becomes necessary
due to a disaster situation where defending in place is not feasible and when the facility cannot continue to support care, treatment and services, the Incident Commander and the jurisdiction fire department may initiate and authorize a vertical
evacuation of the facility. If vertical evacuation becomes necessary, the following protocol will be followed:
Vertical Evacuations
- If a vertical evacuation is required, the patients should be moved vertically down and horizontally away from the affected area(s).
- Once evacuation priorities have been established, the safest route to vertically evacuate patients should be chosen and communicated by the on-scene incident commander. It may be necessary to move patients vertically up and horizontally across
then vertically down depending on the location of the affected areas.
- Holding areas for the patients shall be identified by the on-scene incident commander. These areas should be chosen to keep all the patients from a specific unit together. Units can be mixed but units should not be split between areas if at all
possible.
- UTMB staff from evacuated units should stay with the patients from their respective floor/unit. Once all patients have been evacuated to the holding area, staff shall complete a patient count and check armbands against the census for their unit
to account for all patients who have been evacuated.
Facility Evacuation once the notification by the on-scene incident commander is made to evacuate:
- Visitors - Because the facility does not have a way to track visitors coming and going from the facility there is not a mechanism in place to account for all visitors. Voice annunciators should be used to announce that all visitors should leave
the facility immediately. If a destination for the patients has been identified, the location may also be paged overhead or otherwise communicated to the visitors.
- Ambulatory Patients - Ambulatory patients and their medication, equipment, and pertinent information, including essential clinical and medication-related information shall be moved as directed above to staging area as coordinated by the on-scene
incident commander.
- Admitting staff shall track each patient as they leave the facility based on the current computer census. Patient disposition shall be determined based on the destination.
- The (HICS) Patient Evacuation Tracking Form shall be utilized for patient tracking. When more than two patients are being evacuated, the Master Patient Evacuation Tracking Form shall be completed to gain a master copy of all patients that
were evacuated.
- A designated point of contact for the hospital will establish communications with the Fire Department/EMS On-scene Incident Command Post and provide information on the number of people remaining in the building.
- The Clinical Enterprise Incident Command should notify the Southeast Texas Regional Trauma Advisory Council (SETRAC) Duty Officer (281-822-4444) or the Catastrophic Medical Operations Center (if activated) (713-426-9508) that UTMB is conducting a hospital
evacuation. SETRAC in turn, can:
- Issue an EMResource request to regional hospitals on bed availability in case additional receiving hospitals are needed.
- Mobilize regional ambulances or ambuses to assist with patient transport from initial staging areas to regional receiving hospitals.
- Obtain needed resources such as pediatric bassinets for evacuation transport.
In the event of limited time or ability to evacuate (e.g., rapid storm intensification, traffic or road closures), UTMB will work with the State to fly C130 planes into Scholes Airport for evacuation. In general, we can expect one plane every two
hours that can transport between 30-50 patients. Helicopters could also be involved from the military and contracted air support companies.
Non-Ambulatory Patients and their medication, equipment, and pertinent information, including essential clinical and medication-related information shall be transported by ambulance or another vehicle designed for patient transport as coordinated by the UTMB on-scene incident commander.
UTMB Healthcare Staff may be needed to staff an alternate care site or to assist with the transfer of patients from UTMB to another UTMB facility or outside hospital. UTMB staff members should be tracked by the Health System Incident Command through the Planning Section with assistance from Human Resources.
More information on tracking is found in EM.12.02.07 (EP2). More information on transporting is found in EM.12.02.05 (EP1).
Additional Resource: Texas State Guard can be called in to help evacuate an area.
Additional Resource: UTMB Hurricane Planning for more information on sheltering and evacuating for a hurricane (UTMB's #1 risk).